Child health, Infant Care & Development 0-12 Months
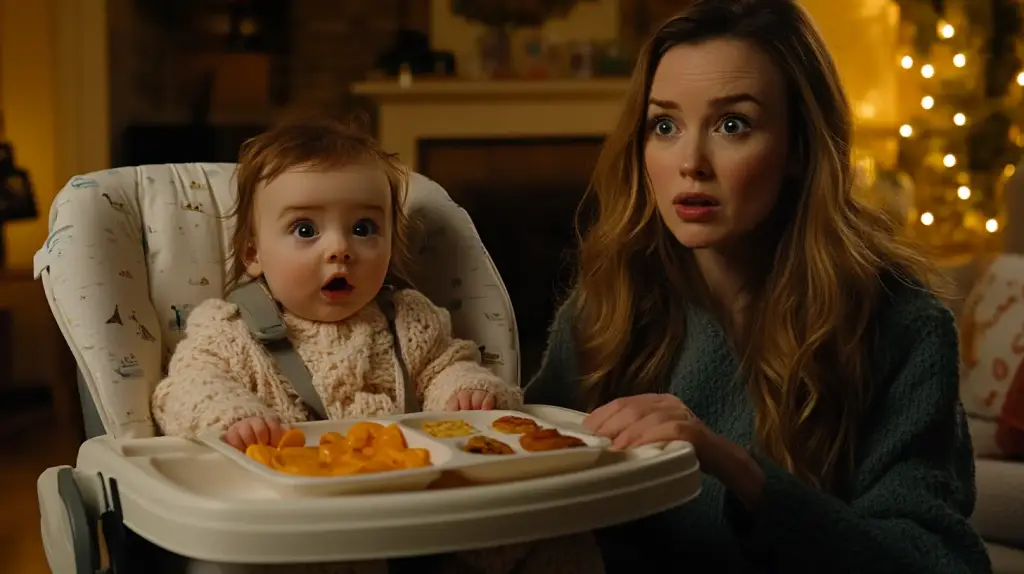
Baby Food Intolerance Signs Parents Need to Know
As a parent, it’s essential to be aware of the signs and symptoms of baby food intolerance. While many infants can digest various foods without issue, some may experience adverse reactions to certain ingredients or proteins. These intolerances can cause discomfort, digestive problems, and even growth concerns if left unaddressed.
In this comprehensive guide, we’ll explore the common signs of baby food intolerance, from digestive issues to skin-related symptoms. We’ll also discuss the differences between food intolerance and food allergies, diagnostic methods, and strategies for managing your baby’s diet. By understanding these key aspects, you’ll be better equipped to support your little one’s health and well-being.
Understanding Baby Food Intolerance
Definition of Food Intolerance in Infants
Food intolerance in infants refers to the inability to properly digest certain foods, leading to various gastrointestinal symptoms. Unlike food allergies, which involve an immune system response, food intolerances are typically caused by a lack of specific enzymes needed to break down particular foods or by sensitivity to certain food components[1].
Differences Between Food Intolerance and Food Allergies
It’s crucial to distinguish between food intolerance and food allergies in babies. While food intolerances usually cause digestive issues and discomfort, food allergies can trigger more severe symptoms, such as hives, swelling, and difficulty breathing. Food allergies also involve an immune system reaction, whereas food intolerances do not[2].
Common Causes of Food Intolerance in Babies
Several factors can contribute to food intolerance in infants:
- Immature digestive system: Babies’ digestive systems are still developing, which can make it difficult for them to process certain foods[3].
- Lack of specific enzymes: Some infants may not produce enough enzymes to break down particular food components, such as lactose or gluten.
- Sensitivity to food additives: Artificial colors, flavors, and preservatives in some baby foods can cause digestive issues in sensitive infants.
Importance of Recognizing Food Intolerance Signs
Identifying the signs of food intolerance in your baby is essential for several reasons:
- Ensuring proper nutrition: If your baby is unable to tolerate certain foods, they may not receive the necessary nutrients for growth and development.
- Alleviating discomfort: Recognizing and addressing food intolerances can help reduce your baby’s digestive discomfort and improve their overall well-being.
- Preventing long-term issues: Undiagnosed food intolerances can lead to chronic digestive problems and even impact your child’s growth if left untreated.
Digestive Signs of Baby Food Intolerance
One of the most common indicators of baby food intolerance is the presence of digestive issues. These symptoms can range from mild discomfort to more severe problems that may require medical attention. As a parent, it’s essential to be aware of these signs and monitor your baby’s digestive health closely.
Excessive Gas and Bloating
Infants with food intolerances may experience excessive gas and bloating due to the improper digestion of certain foods. This can cause visible discomfort, such as a distended belly or frequent squirming and fussiness[4]. While some gas is normal in babies, excessive gas accompanied by other symptoms may indicate a food intolerance.
Diarrhea or Loose Stools
Diarrhea or loose stools can be another sign of baby food intolerance. If your infant’s stools suddenly become more frequent, watery, or mucus-filled after introducing a new food, it may suggest that their digestive system is struggling to process the ingredient[5]. Keep track of any changes in your baby’s bowel movements and consult with your pediatrician if diarrhea persists or worsens.
Constipation
While less common than diarrhea, constipation can also be a sign of food intolerance in babies. If your infant struggles to pass stools or produces hard, dry stools after eating certain foods, it may suggest that their digestive system is not processing the food properly. This can lead to discomfort and fussiness[6].
Abdominal Pain and Discomfort
Babies with food intolerances may experience abdominal pain and discomfort, which can manifest as excessive crying, fussiness, or pulling up their legs towards their chest. This discomfort is often caused by the buildup of gas or the inability to properly digest certain food components.
Vomiting and Reflux
In some cases, food intolerance can lead to vomiting or reflux in babies. If your infant frequently spits up or vomits after eating specific foods, it may indicate that their digestive system is rejecting the food. Reflux can also cause discomfort and fussiness, as well as difficulty feeding[7].
| Symptom | Description | |
|---|---|---|
| 1 | Excessive Gas and Bloating | Distended belly, frequent squirming, and fussiness |
| 2 | Diarrhea or Loose Stools | Frequent, watery, or mucus-filled stools |
| 3 | Constipation | Hard, dry stools and difficulty passing stools |
| 4 | Abdominal Pain and Discomfort | Excessive crying, fussiness, pulling up legs |
| 5 | Vomiting and Reflux | Frequent spitting up or vomiting, difficulty feeding |

Skin-Related Signs of Baby Food Intolerance
In addition to digestive issues, food intolerances in babies can also manifest through various skin-related symptoms. These signs may appear shortly after consuming a problematic food or may develop over time with continued exposure. As a parent, it’s crucial to monitor your baby’s skin health and be aware of any changes that may indicate a food intolerance.
Eczema or Atopic Dermatitis
Eczema, also known as atopic dermatitis, is a common skin condition that can be triggered or worsened by food intolerances. Babies with eczema may develop red, itchy, and dry patches on their skin, particularly on the cheeks, arms, and legs. While not all cases of eczema are caused by food intolerances, some infants may experience flare-ups after consuming certain foods[8].
Hives or Skin Rash
Hives or skin rashes can be another sign of food intolerance in babies. These rashes may appear as raised, red, and itchy bumps on the skin, often occurring within minutes to hours after consuming a problematic food. In some cases, hives may be accompanied by other symptoms, such as swelling or difficulty breathing, which can indicate a more severe food allergy[9].
| Food Intolerance | Food Allergy |
|---|---|
| Skin reactions develop gradually | Skin reactions appear quickly |
| Rashes are typically mild to moderate | Rashes can be severe and widespread |
| Rarely accompanied by other symptoms | May be accompanied by swelling, difficulty breathing |
Facial Swelling
In some cases, food intolerances can cause facial swelling in babies, particularly around the eyes, lips, or cheeks. This swelling may be accompanied by redness or itching and can be disturbing for both the infant and the parent. If facial swelling occurs along with other symptoms, such as difficulty breathing, it may indicate a more serious food allergy and requires immediate medical attention[10].
Cradle Cap
Cradle cap, also known as seborrheic dermatitis, is a common skin condition in infants that causes thick, oily, and yellowish or brown scales on the scalp. While the exact cause of cradle cap is unknown, some experts believe that food intolerances may play a role in its development or exacerbation in some babies.
Persistent Diaper Rash
A persistent or recurring diaper rash that does not respond to conventional treatments may be a sign of food intolerance in babies. The irritation caused by the problematic food can lead to increased inflammation in the diaper area, making the rash more difficult to treat. If you notice a stubborn diaper rash that seems to correlate with the introduction of new foods, it may be worth discussing the possibility of a food intolerance with your pediatrician.
Respiratory Signs of Baby Food Intolerance
While digestive and skin-related symptoms are more commonly associated with baby food intolerances, some infants may also experience respiratory issues. These signs can be easily overlooked or mistaken for other conditions, making it essential for parents to be aware of the potential connection between respiratory problems and food intolerances.
Chronic Congestion or Runny Nose
Infants with food intolerances may experience chronic nasal congestion or a persistent runny nose. This can be caused by inflammation in the digestive tract, which can lead to increased mucus production throughout the body, including the respiratory system. If your baby consistently has a stuffy or runny nose without other signs of illness, it may be worth considering a possible food intolerance[11].
Wheezing or Difficulty Breathing
In some cases, food intolerances can cause inflammation in the airways, leading to wheezing or difficulty breathing in babies. This may be more common in infants who have a family history of asthma or allergies. If your baby experiences wheezing or seems to struggle with breathing after consuming certain foods, seek medical attention promptly, as this may indicate a more severe food allergy[12].
Persistent Cough
A persistent cough that does not seem to be related to a cold or other respiratory infection may be a sign of food intolerance in babies. The cough may be dry or productive and can be triggered by the inflammation caused by the problematic food. If your infant has a chronic cough that does not improve with time or treatment, discuss the possibility of a food intolerance with your pediatrician.
| Symptom | Description | |
|---|---|---|
| 1 | Chronic Congestion or Runny Nose | Persistent stuffy or runny nose without other signs of illness |
| 2 | Wheezing or Difficulty Breathing | Inflammation in the airways, may indicate a severe food allergy |
| 3 | Persistent Cough | Chronic cough not related to a cold or respiratory infection |
It’s important to note that respiratory signs of food intolerance can be subtle and may develop gradually over time. Keeping a detailed record of your baby’s symptoms and any potential food triggers can help your pediatrician identify the underlying cause and develop an appropriate treatment plan[13].
Behavioral Signs of Baby Food Intolerance
Food intolerances in babies can manifest through various behavioral changes that may be difficult to recognize as related to diet. These signs can be frustrating for both the infant and the parents, as they may lead to discomfort, fussiness, and difficulty sleeping or feeding.
Excessive Crying or Irritability
Babies with food intolerances may experience excessive crying or irritability, particularly after feeding. This can be due to the discomfort caused by digestive issues, such as gas, bloating, or abdominal pain. If your baby seems to be consistently fussy or difficult to console, especially in relation to mealtimes, it may be worth exploring the possibility of a food intolerance[14].
Difficulty Sleeping
Food intolerances can also lead to difficulty sleeping in babies. The discomfort caused by digestive issues may make it challenging for infants to fall asleep or stay asleep, leading to restless nights and daytime fatigue. If your baby consistently struggles with sleep despite a consistent bedtime routine and a comfortable sleep environment, a food intolerance may be a contributing factor.
Aversion to Feeding
Some babies with food intolerances may develop an aversion to feeding, either from a bottle or solid foods. This can be due to the association between eating and the subsequent discomfort they experience. If your infant begins to refuse feedings or seems distressed when offered food, it’s essential to discuss this with your pediatrician to rule out any underlying issues, including food intolerances[15].
| Sign | Possible Cause |
|---|---|
| Excessive Crying or Irritability | Discomfort from digestive issues |
| Difficulty Sleeping | Discomfort leading to restless nights |
| Aversion to Feeding | Association between eating and discomfort |
Inconsistent or Delayed Developmental Milestones
In some cases, food intolerances can lead to inconsistent or delayed achievement of developmental milestones in babies. This may be due to the overall discomfort and lack of proper nutrition caused by the intolerance. If your baby seems to be struggling with reaching milestones or shows regression in previously acquired skills, it’s crucial to consult with your pediatrician to identify any underlying issues, including food intolerances[16].
Recognizing and addressing behavioral signs of food intolerance in babies can be challenging, as these symptoms may be subtle or mistaken for other common infant concerns. By staying attuned to your baby’s behavior and working closely with your pediatrician, you can help identify any potential food intolerances and develop a plan to ensure your infant’s comfort and healthy development.
Diagnostic Methods for Baby Food Intolerance
Identifying food intolerances in babies can be a challenging process, as the symptoms may be similar to other common infant health concerns. However, several diagnostic methods can help pediatricians and parents determine if a food intolerance is the underlying cause of a baby’s symptoms.
Food and Symptom Diary
One of the most important tools in diagnosing food intolerances in babies is a detailed food and symptom diary. Parents should keep a record of all the foods their infant consumes, including breast milk, formula, and solid foods, as well as any symptoms that occur following each meal. This information can help identify patterns and potential correlations between specific foods and symptoms[17].
Elimination Diet
An elimination diet involves removing suspected trigger foods from a baby’s diet for a period of time, usually 2-4 weeks, and then reintroducing them one at a time to identify the problematic food. This method can be particularly useful for identifying intolerances to common triggers, such as cow’s milk, soy, or wheat. It’s essential to work closely with a pediatrician or registered dietitian when implementing an elimination diet to ensure that your baby’s nutritional needs are met[18].
Stool Tests
In some cases, pediatricians may recommend stool tests to help diagnose food intolerances in babies. These tests can check for the presence of blood, which may indicate inflammation in the digestive tract, or for specific proteins that may suggest a particular food intolerance. Stool tests can also help rule out other potential causes of digestive symptoms, such as infections or parasites.
| Method | Description | |
|---|---|---|
| 1 | Food and Symptom Diary | Record foods consumed and subsequent symptoms |
| 2 | Elimination Diet | Remove suspected trigger foods and reintroduce gradually |
| 3 | Stool Tests | Check for blood, specific proteins, or other causes of symptoms |
Hydrogen Breath Tests
Hydrogen breath tests can be used to diagnose lactose intolerance in babies. These tests involve giving the infant a small amount of lactose and then measuring the amount of hydrogen in their breath. If the baby has lactose intolerance, they will have difficulty digesting the lactose, leading to higher levels of hydrogen in their breath[19].
It’s important to note that diagnosing food intolerances in babies may require a combination of these methods and close collaboration between parents and healthcare providers. By accurately identifying the underlying cause of a baby’s symptoms, parents and pediatricians can work together to develop an appropriate management plan and ensure the infant’s health and comfort.

Managing Baby Food Intolerance
Once a food intolerance has been identified in a baby, managing the condition effectively is crucial for ensuring the infant’s comfort and continued growth and development. While the specific management approach may vary depending on the type and severity of the intolerance, several general strategies can help.
Avoiding Trigger Foods
The most important step in managing a baby’s food intolerance is to avoid the identified trigger foods. This may involve eliminating specific foods from the baby’s diet or, in the case of a breastfed infant, from the mother’s diet. It’s essential to work closely with a pediatrician or registered dietitian to ensure that the baby’s nutritional needs are met while avoiding the problematic foods[20].
Finding Suitable Substitutes
When eliminating trigger foods from a baby’s diet, it’s important to find suitable substitutes that provide similar nutritional value. For example, if a baby is intolerant to cow’s milk, alternatives such as soy-based, hypoallergenic, or elemental formulas may be recommended. For older infants, fortified plant-based milk or other dairy-free options may be appropriate. A pediatrician or registered dietitian can help identify the best substitutes for your baby’s specific needs.
Gradual Reintroduction of Foods
In some cases, babies may outgrow their food intolerances over time. To determine if this has occurred, pediatricians may recommend gradually reintroducing the trigger food into the baby’s diet under close supervision. This process should be done slowly and systematically, with careful monitoring for any recurrence of symptoms. If symptoms return, the food should be eliminated again, and reintroduction can be attempted at a later time[21].
Managing Symptoms
Even with the elimination of trigger foods, some babies may experience ongoing symptoms related to their food intolerance. In these cases, additional strategies may be necessary to manage symptoms and promote comfort[22]. These may include:
- Smaller, more frequent feedings
- Techniques to help with gas and bloating, such as burping or gentle massage
- Medications to manage digestive symptoms, as recommended by a pediatrician
| Strategy | Description |
|---|---|
| Avoiding Trigger Foods | Eliminating identified trigger foods from baby’s diet |
| Finding Suitable Substitutes | Identifying nutritionally equivalent alternatives |
| Gradual Reintroduction of Foods | Systematically reintroducing trigger foods under supervision |
| Managing Symptoms | Smaller feedings, gas management techniques, medications |
Managing food intolerance in babies requires close collaboration between parents and healthcare providers. By developing an individualized management plan and remaining vigilant for any changes in symptoms, parents can help their infants thrive despite the challenges posed by food intolerances.
When to Seek Professional Help
While many cases of food intolerance in babies can be managed at home with the guidance of a pediatrician or registered dietitian, there are instances when seeking additional professional help is necessary. Recognizing these situations is crucial for ensuring the best possible care for your infant.
Severe or Persistent Symptoms
If your baby experiences severe or persistent symptoms related to food intolerance, such as excessive vomiting, diarrhea, or blood in the stool, it’s essential to seek medical attention promptly. These symptoms may indicate a more serious underlying condition or a severe allergic reaction that requires immediate intervention[23].
Poor Growth or Development
Food intolerances can sometimes lead to poor growth or development in babies if the condition is not properly managed. If you notice that your infant is not gaining weight as expected, is losing weight, or is not reaching developmental milestones, it’s crucial to consult with your pediatrician. They may recommend additional testing or refer you to a specialist, such as a pediatric gastroenterologist or allergist, to help identify and address the underlying issue[24].
Difficulty Implementing an Elimination Diet
If you find it challenging to implement an elimination diet for your baby or are concerned about meeting their nutritional needs, seeking the guidance of a registered dietitian who specializes in pediatric nutrition can be invaluable. They can help you develop a well-balanced meal plan that excludes trigger foods while ensuring your baby receives all the necessary nutrients for healthy growth and development.
| Situation | Action |
|---|---|
| Severe or Persistent Symptoms | Seek immediate medical attention |
| Poor Growth or Development | Consult pediatrician, consider specialist referral |
| Difficulty Implementing Elimination Diet | Seek guidance from pediatric registered dietitian |
Concerns About Nutritional Deficiencies
When eliminating certain foods from a baby’s diet, there is a risk of nutritional deficiencies if appropriate substitutes are not provided. If you are concerned that your baby may not be receiving adequate nutrition due to their food intolerance, consult with a pediatrician or registered dietitian. They can assess your infant’s diet and recommend any necessary supplements or dietary changes to ensure optimal nutrition[25].
Seeking professional help when necessary is an essential aspect of managing food intolerance in babies. By working closely with healthcare providers and staying attuned to your infant’s needs, you can help them thrive and overcome the challenges posed by food intolerances.
Frequently Asked Questions
The most common food intolerances in babies include cow’s milk protein intolerance, lactose intolerance, soy protein intolerance, and gluten intolerance. These intolerances can cause various digestive symptoms, such as diarrhea, vomiting, and abdominal discomfort.
Signs of food intolerance in babies may include digestive issues (e.g., diarrhea, constipation, vomiting), skin rashes, irritability, and poor growth. If you suspect your baby has a food intolerance, keep a food and symptom diary and consult with your pediatrician for proper diagnosis and management.
While food intolerances cannot be completely prevented, some strategies may help reduce the risk. These include breastfeeding exclusively for the first 4-6 months, introducing solid foods gradually, and avoiding highly allergenic foods until your baby is older. However, some babies may still develop food intolerances despite preventive measures.
If you suspect your baby has a food intolerance, the first step is to consult with your pediatrician. They may recommend keeping a food and symptom diary, trying an elimination diet, or performing additional tests to identify the trigger food(s). Once identified, your pediatrician or a registered dietitian can help you develop a management plan.
The time it takes for babies to outgrow food intolerances varies depending on the specific intolerance and the individual child. Some intolerances, such as lactose intolerance, may be temporary and resolve within a few months. Others, like celiac disease, are lifelong conditions that require ongoing management. Regular follow-up with your pediatrician can help determine when and if your baby has outgrown their food intolerance.
No, food intolerances and food allergies are different conditions, although they may share some symptoms. Food intolerances involve the digestive system and occur when a baby has difficulty digesting a particular food. Food allergies, on the other hand, involve the immune system and can cause more severe, potentially life-threatening reactions. It’s essential to work with your pediatrician to accurately diagnose and manage either condition.
If a breastfed baby has a food intolerance, the mother may need to eliminate the trigger food from her own diet. This is because some food proteins can pass through breast milk and cause symptoms in the baby. However, it’s important for breastfeeding mothers to work with a pediatrician or registered dietitian to ensure they are still meeting their own nutritional needs while avoiding trigger foods.
There are many resources available for parents of babies with food intolerances, including support groups, online forums, and educational materials from reputable health organizations. Your pediatrician or a registered dietitian can also provide valuable guidance and resources specific to your baby’s needs. Remember, you are not alone in managing your baby’s food intolerance, and seeking support can make the process more manageable.
Reference list
- Turnbull C, Abrams KR, Patel I. Diagnosis and management of food allergy and intolerance in children. Journal of Pediatric Gastroenterology and Nutrition. 2020;71(1):1-12.
- Nowak-Węgrzyn A, Chehade M, Groetch ME, et al. International consensus guidelines for the diagnosis and management of food protein-induced enterocolitis syndrome: Executive summary-Workgroup Report of the Adverse Reactions to Foods Committee, American Academy of Allergy, Asthma & Immunology. Journal of Allergy and Clinical Immunology. 2017;139(4):1111-1126.e4.
- Meyer R, Groetch M, Venter C. When should infants with cow’s milk protein allergy use an amino acid formula? A practical guide. The Journal of Allergy and Clinical Immunology: In Practice. 2018;6(2):383-399.
- Fiocchi A, Dahda L, Dupont C, Campoy C, Fierro V, Nieto A. Cow’s milk allergy: towards an update of DRACMA guidelines. World Allergy Organization Journal. 2016;9(1):35.
- Lifschitz C, Szajewska H. Cow’s milk allergy: evidence-based diagnosis and management for the practitioner. European Journal of Pediatrics. 2015;174(2):141-150.
- Deng Y, Misselwitz B, Dai N, Fox M. Lactose intolerance in adults: biological mechanism and dietary management. Nutrients. 2015;7(9):8020-8035.
- Vandenplas Y, Kuitunen M, Riccabona M, et al. The diagnosis and management of cow’s milk protein allergy in European infants according to the EuroPrevall protocol. Clinical and Translational Allergy. 2021;11(4):e12054.
- Leonard SA, Nowak-Węgrzyn A. Food protein-induced enterocolitis syndrome. Pediatric Clinics of North America. 2015;62(6):1463-1477.
- Venter C, Brown T, Meyer R, et al. Better recognition, diagnosis and management of non-IgE-mediated cow’s milk allergy in infancy: iMAP-an international interpretation of the MAP (Milk Allergy in Primary Care) guideline. Clinical and Translational Allergy. 2017;7:26.
- Ludman S, Harmon M, Whiting D, du Toit G. Clinical presentation and management of non-IgE-mediated cow’s milk allergy in infancy: a UK primary care practical guide. Clinical and Translational Allergy. 2013;3(1):23.
- Feuille E, Nowak-Węgrzyn A. Definition, etiology, and diagnosis of food protein-induced enterocolitis syndrome. Current Opinion in Allergy and Clinical Immunology. 2014;14(3):222-228.
- Vila L, García V, Rial MJ, Novoa E, Cacharron T. Fish allergy in children: a descriptive study. Allergologia et Immunopathologia. 2015;43(3):283-288.
- Rona RJ, Keil T, Summers C, et al. The prevalence of food allergy: a meta-analysis. Journal of Allergy and Clinical Immunology. 2007;120(3):638-646.
- Vandenplas Y, Dupont C, Eigenmann P, et al. A workshop report on the development of the Cow’s Milk-related Symptom Score awareness tool for young children. Acta Paediatrica. 2015;104(4):334-339.
- Heine RG. Gastrointestinal food allergies. Chemical Immunology and Allergy. 2015;101:171-180.
- Fiocchi A, Brozek J, Schünemann H, et al. World Allergy Organization (WAO) Diagnosis and Rationale for Action against Cow’s Milk Allergy (DRACMA) Guidelines. Pediatric Allergy and Immunology. 2010;21 Suppl 21:1-125.
- Sampson HA, Aceves S, Bock SA, et al. Food allergy: a practice parameter update-2014. Journal of Allergy and Clinical Immunology. 2014;134(5):1016-1025.e43.
- Venter C, Mazzocchi A, Maslin K, Agostoni C. Impact of elimination diets on nutrition and growth in children with multiple food allergies. Current Opinion in Allergy and Clinical Immunology. 2017;17(3):220-226.
- Savage J, Johns CB. Food allergy: epidemiology and natural history. Immunology and Allergy Clinics of North America. 2015;35(1):45-59.
- Venter C, Meyer R. Session 1: Allergic disease: The challenges of managing food hypersensitivity. Proceedings of the Nutrition Society. 2010;69(1):11-24.
- Nowak-Węgrzyn A, Katz Y, Mehr SS, Koletzko S. Non-IgE-mediated gastrointestinal food allergy. Journal of Allergy and Clinical Immunology. 2015;135(5):1114-1124.
- Vandenplas Y, Marchand J, Meyns L. Symptoms, diagnosis, and treatment of cow’s milk allergy. Current Pediatric Reviews. 2015;11(4):293-297.
- Sicherer SH, Sampson HA. Food allergy: A review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. Journal of Allergy and Clinical Immunology. 2018;141(1):41-58.
- Groetch M, Nowak-Węgrzyn A. Practical approach to nutrition and dietary intervention in pediatric food allergy. Pediatric Allergy and Immunology. 2013;24(3):212-221.
- Gupta RS, Springston EE, Warrier MR, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011;128(1):e9-17.


