Joint Diseases, Metabolism
Best Ways to Ice Sore Joints for Maximum Relief
Joint pain is a common complaint that can significantly impact daily activities and quality of life. Whether caused by injury, overuse, or chronic conditions like arthritis, finding effective ways to manage joint discomfort is crucial for maintaining mobility and well-being. Among the various treatment options available, icing has long been recognized as a simple yet powerful method for reducing inflammation, numbing pain, and promoting healing in sore joints.
In this comprehensive guide, we will explore the best ways to ice sore joints for maximum relief. From understanding the benefits of cold therapy to mastering specific icing techniques for different joints, you’ll discover how to effectively incorporate icing into your pain management routine. We’ll also discuss important precautions, complementary strategies, and when to seek medical attention for persistent joint pain. By the end of this article, you’ll be equipped with the knowledge and tools needed to find relief and take control of your joint health.
Understanding Joint Pain and the Benefits of Icing
Joint pain is a prevalent issue that affects millions of people worldwide. It can be caused by various factors, including injury, overuse, and chronic conditions such as osteoarthritis or rheumatoid arthritis. Regardless of the underlying cause, joint pain can significantly impact an individual’s ability to perform daily activities and enjoy a high quality of life.
Common causes of joint pain
Some of the most common causes of joint pain include:
- Acute injuries, such as sprains, strains, or fractures
- Overuse or repetitive stress on a particular joint
- Age-related wear and tear, leading to conditions like osteoarthritis
- Inflammatory conditions, such as rheumatoid arthritis or gout
- Infections or illnesses that affect joint health
How cold therapy works to reduce inflammation and pain
Icing, or cold therapy, is a simple and effective way to manage joint pain and inflammation. When applied to the affected area, cold temperatures cause blood vessels to constrict, reducing blood flow and limiting the accumulation of fluid in the surrounding tissues[1]. This process helps to minimize swelling, inflammation, and pain in the affected joint.
When to use ice for joint pain relief
Icing is most effective when used during the acute phase of an injury or flare-up, typically within the first 24 to 48 hours[2]. It can also be used to manage chronic joint pain, especially after physical activity or when experiencing a particularly painful episode. However, it’s essential to follow proper guidelines and not overdo it, as excessive icing can potentially damage skin or nerves.
| Acute Injury | Chronic Pain | |
|---|---|---|
| Duration | 15-20 minutes | 10-15 minutes |
| Frequency | Every 1-2 hours | 2-3 times daily |
Precautions and contraindications for icing joints
While icing is generally safe for most people, there are some precautions and contraindications to keep in mind. Individuals with circulatory issues, nerve damage, or reduced sensation in the affected area should consult with a healthcare provider before using cold therapy[3]. Additionally, it’s crucial to protect the skin from direct contact with ice, as this can cause frostbite or tissue damage.
Preparing for Icing Your Joints
Before you begin icing your sore joints, it’s essential to gather the necessary materials and create a comfortable setup. Taking the time to prepare properly will ensure that your icing sessions are effective and enjoyable.
Gathering necessary materials
To get started, you’ll need the following items:
- Ice packs or bags of frozen vegetables
- Clean towels or cloths
- Compression wraps or elastic bandages
- A comfortable place to sit or lie down
If you opt for reusable ice packs, make sure to have several on hand so you can rotate them as needed. Bags of frozen vegetables, such as peas or corn, can also be used as a convenient and conforming alternative to traditional ice packs[4].
Creating a comfortable setup for icing sessions
Find a quiet, comfortable spot where you can relax while icing your joints. This could be a couch, recliner, or bed. Place a towel or protective layer over the surface to catch any moisture from the melting ice. Arrange your ice packs, towels, and compression wraps within easy reach.
Timing and frequency of icing for optimal results
The duration and frequency of your icing sessions will depend on whether you are treating an acute injury or managing chronic joint pain. For acute injuries, aim for 15-20 minute sessions every 1-2 hours during the first 24-48 hours[5]. For chronic pain, 10-15 minute sessions 2-3 times per day may be sufficient.
| Duration | Frequency | |
|---|---|---|
| Acute Injury | 15-20 minutes | Every 1-2 hours |
| Chronic Pain | 10-15 minutes | 2-3 times per day |
Protecting skin from direct contact with ice
Always place a thin towel or cloth between the ice pack and your skin to prevent frostbite or tissue damage. Never apply ice directly to the skin, as this can cause harm. If you experience numbness, tingling, or discomfort during your icing session, remove the ice pack immediately and allow the area to warm up gradually[6].
By gathering the right materials, creating a comfortable environment, and following proper timing and safety guidelines, you’ll be well-prepared to start icing your joints effectively.

Different Methods of Icing Sore Joints
There are several ways to apply ice to sore joints, each with its own benefits and advantages. Experimenting with different methods can help you find the one that works best for your specific needs and preferences.
Using traditional ice packs or bags of frozen vegetables
The most common method of icing joints is using traditional ice packs or bags of frozen vegetables. These options are easily accessible, affordable, and can be molded to fit the contours of the affected joint. When using an ice pack, be sure to wrap it in a thin towel before applying it to the skin to prevent direct contact[7].
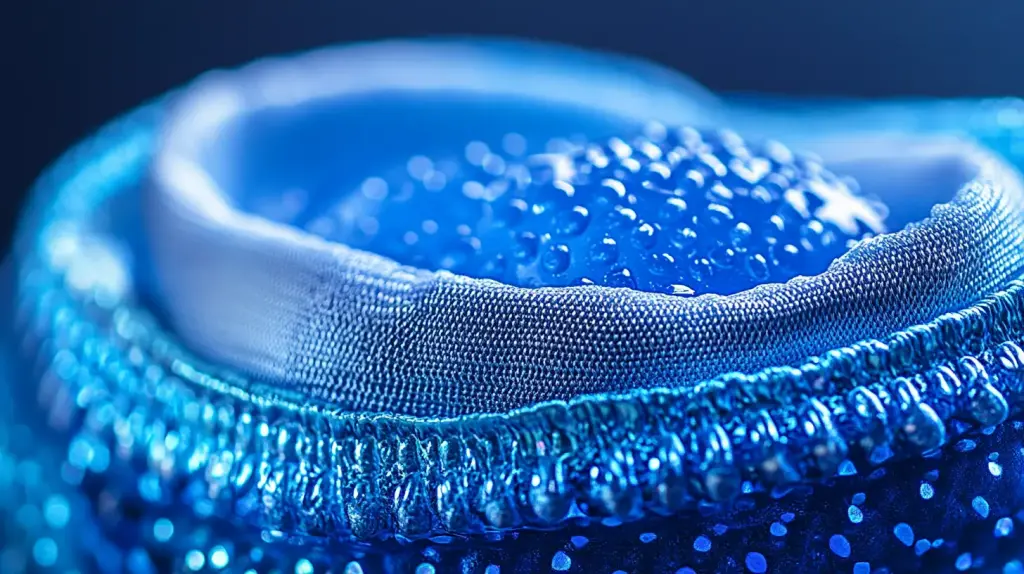
Applying cold compression wraps for targeted relief
Cold compression wraps are another effective option for icing sore joints. These wraps combine the benefits of cold therapy with compression, which helps to reduce swelling and inflammation. Many cold compression wraps are designed to fit specific joints, such as the knee, elbow, or ankle, allowing for targeted relief[8].
- To use a cold compression wrap, simply place it in the freezer for the recommended amount of time, then apply it to the affected joint.
- Some wraps come with adjustable straps or Velcro closures, allowing you to customize the level of compression.
- Be sure to follow the manufacturer’s instructions for proper use and care of the wrap.
Trying ice massage for specific joint pain
Ice massage is a technique that involves applying ice directly to the skin in a circular motion. This method is particularly useful for targeting specific areas of joint pain, such as the kneecap or shoulder. To perform an ice massage, follow these steps:
| Step | Description |
|---|---|
| 1 | Fill a paper cup with water and freeze it until solid |
| 2 | Peel back the top of the cup to expose the ice |
| 3 | Massage the affected area with the ice in a circular motion |
| 4 | Continue for 5-10 minutes, or until the area feels numb |
Alternating between ice and heat therapy
While icing is the primary focus for acute injuries and inflammation, alternating between cold and heat therapy can be beneficial for chronic joint pain or stiffness. This method, known as contrast therapy, involves applying ice for several minutes, followed by heat for a similar duration. The alternating temperatures help to stimulate blood flow and reduce pain[9].
Icing Techniques for Specific Joints
Different joints require unique approaches to icing due to their varying anatomical structures and surrounding soft tissues. Understanding the specific techniques for each joint can help maximize pain relief and reduce inflammation more effectively.
Icing the knee joint effectively
The knee is a complex joint that often experiences pain from injuries, arthritis, or overuse. When icing the knee, it’s crucial to cover the entire joint area while protecting the skin. Use a large ice pack or cold compression wrap that can conform to the knee’s shape[10]. Position yourself comfortably, either sitting or lying down, with the knee slightly elevated.
- Use a barrier cloth between the ice pack and skin
- Apply ice for 15-20 minutes at a time
- Repeat icing every 2-3 hours during acute pain
- Combine with gentle compression for maximum relief
Applying ice to sore shoulder joints
Shoulder joint pain can be particularly challenging due to the joint’s complex range of motion. When icing a sore shoulder, use a smaller, more flexible ice pack that can target the specific area of discomfort[11]. Ensure you can comfortably position the ice pack while maintaining some arm mobility.
| Position | Sitting | Lying Down |
|---|---|---|
| Recommended Technique | Ice pack on shoulder | Ice pack behind shoulder |
| Duration | 15 minutes | 15-20 minutes |
Relieving hip joint pain with cold therapy
Hip joint pain requires a strategic approach to icing. The deep location of the hip joint means you’ll need to use larger ice packs or cold compression wraps that can cover a broader area. Pay special attention to the specific location of your pain, whether it’s in the front, side, or back of the hip[12].
Icing techniques for ankle and wrist joints
Smaller joints like ankles and wrists benefit from more precise icing methods. For these areas, consider using smaller ice packs or even ice massage techniques. Wrap the ice in a thin towel and gently move it around the joint, being careful not to apply direct pressure that might cause additional discomfort.

Combining Icing with Other Pain Relief Strategies
While icing is an effective method for managing joint pain, combining it with other pain relief strategies can provide even greater benefits. By taking a holistic approach to pain management, you can address the various factors contributing to your discomfort and improve your overall quality of life.
Using over-the-counter pain medications
Over-the-counter pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen, can help reduce inflammation and relieve pain when used in conjunction with icing[13]. Always follow the recommended dosage instructions and consult with your healthcare provider if you have any concerns or pre-existing medical conditions.
Incorporating gentle exercise and stretching
Engaging in gentle exercise and stretching can help improve joint mobility, reduce stiffness, and promote healing. Low-impact activities like swimming, yoga, or tai chi are excellent options for individuals with joint pain. When combined with regular icing, these exercises can help you maintain flexibility and strength in the affected joints[14].
- Start with short, gentle sessions and gradually increase duration and intensity
- Focus on exercises that target the affected joint(s)
- Stretch before and after exercise to prevent further injury
- Listen to your body and stop if you experience pain
Trying heat therapy for chronic joint stiffness
While icing is the go-to treatment for acute joint pain and inflammation, heat therapy can be beneficial for chronic joint stiffness and muscle tension. Applying heat to the affected area can help improve blood flow, relax muscles, and reduce pain. Consider alternating between icing and heat therapy for optimal results[15].
| Icing | Heat Therapy | |
|---|---|---|
| Best for | Acute pain, inflammation | Chronic stiffness, muscle tension |
| Duration | 15-20 minutes | 15-20 minutes |
| Frequency | Every 2-3 hours | 2-3 times daily |
Exploring complementary therapies
Complementary therapies, such as acupuncture, massage, or chiropractic care, may provide additional relief when used alongside icing and other pain management strategies. These therapies can help address underlying imbalances, reduce stress, and promote overall well-being. Be sure to consult with qualified practitioners and inform them of your existing treatment plan.
Adapting Icing Methods for Chronic Joint Conditions
Chronic joint conditions such as osteoarthritis, rheumatoid arthritis, and fibromyalgia require a more nuanced approach to icing and pain management. Understanding how to adapt cold therapy for long-term joint issues can help improve overall symptom management and quality of life.
Understanding chronic joint inflammation
Chronic joint conditions involve persistent inflammation that differs from acute injury-related inflammation. For individuals with ongoing joint problems, icing must be approached with greater care and consideration[16]. The goal is to manage pain and reduce inflammation without causing additional stress to the joints.
- Consult with a rheumatologist or specialist
- Develop a personalized icing strategy
- Monitor joint response to cold therapy
- Adjust techniques based on individual symptoms
Modifying icing frequency for long-term management
Unlike acute injuries, chronic joint conditions require a more measured approach to icing. Patients should focus on shorter, more frequent icing sessions that provide relief without overwhelming the joint’s natural healing processes[17]. The key is to find a balance that reduces pain and inflammation without causing additional stress.
| Condition | Duration | Frequency |
|---|---|---|
| Osteoarthritis | 10-15 minutes | 2-3 times daily |
| Rheumatoid Arthritis | 10-15 minutes | As needed during flare-ups |
| Fibromyalgia | 5-10 minutes | When pain is most intense |
Alternative cold therapy techniques for sensitive joints
Individuals with chronic joint conditions often have more sensitive joints that may not tolerate traditional icing methods. Consider exploring alternative approaches such as:
- Gel-based cold packs with softer, more flexible materials
- Cooling wraps designed for specific joint areas
- Partial icing techniques that target specific pain points
Monitoring and adjusting cold therapy
Chronic joint conditions require continuous monitoring and adjustment of pain management strategies. Pay close attention to how your joints respond to icing, and be prepared to modify your approach as symptoms change[18]. Keep a pain journal to track the effectiveness of your cold therapy technique and discuss findings with your healthcare provider.

Preventing Joint Pain and Injury
Preventing joint pain and injury is crucial for maintaining long-term joint health and mobility. By implementing proactive strategies, you can reduce the risk of joint-related issues and minimize the need for extensive treatment.
Maintaining a healthy lifestyle
A comprehensive approach to joint health begins with overall lifestyle choices. Maintaining a healthy weight, eating a balanced diet rich in anti-inflammatory foods, and staying hydrated can significantly impact joint wellness[19]. Regular exercise and proper nutrition play key roles in supporting joint function and preventing potential injuries.
- Maintain a healthy body weight
- Consume omega-3 rich foods
- Stay hydrated
- Practice regular low-impact exercise
Implementing proper exercise techniques
Correct exercise techniques are essential for preventing joint stress and potential injuries. Focus on exercises that strengthen the muscles surrounding your joints, improve flexibility, and promote overall joint stability[20]. Consult with a fitness professional or physical therapist to develop a personalized exercise routine.
| Exercise Type | Benefits | Frequency |
|---|---|---|
| Swimming | Low-impact, full-body workout | 2-3 times per week |
| Yoga | Improves flexibility and strength | 3-4 times per week |
| Cycling | Cardiovascular health, low joint stress | 2-3 times per week |
Using protective gear and equipment
When participating in sports or physical activities, use appropriate protective gear and equipment to minimize joint stress. This includes wearing supportive shoes, using knee or elbow pads during high-impact activities, and selecting equipment that provides proper support and cushioning[21].
Recognizing early signs of joint stress
Early detection of potential joint issues can prevent more serious injuries. Pay attention to persistent pain, swelling, reduced range of motion, or discomfort during physical activities. If you experience recurring joint symptoms, consult a healthcare professional for a comprehensive evaluation and personalized advice.
Creating ergonomic work and living environments
Design your workspace and living areas to minimize joint strain. Use ergonomic chairs, adjustable workstations, and proper lifting techniques to reduce unnecessary stress on your joints. Consider using supportive cushions, maintaining good posture, and taking regular breaks during prolonged sitting or repetitive activities.
When to Seek Medical Attention for Joint Pain
While many joint issues can be managed with self-care techniques, some symptoms require professional medical evaluation. Understanding when to seek medical attention is crucial for preventing long-term damage and addressing potentially serious underlying conditions.
Identifying serious joint pain warning signs
Certain joint pain symptoms indicate the need for immediate medical attention. These warning signs suggest potential serious conditions that require professional assessment[22]. Recognizing these indicators can help prevent further complications and ensure timely treatment.
- Sudden, severe joint pain
- Joint swelling that does not resolve
- Inability to move the joint
- Fever accompanying joint pain
- Visible joint deformity
Understanding chronic joint pain progression
Chronic joint conditions require careful monitoring and professional guidance. If your joint pain persists or worsens despite self-care treatments, consulting a healthcare specialist becomes essential[23]. Early intervention can prevent further joint deterioration and improve long-term outcomes.
| Symptom Duration | Recommended Action |
|---|---|
| Pain lasting over 2 weeks | Schedule primary care consultation |
| Recurring joint inflammation | Refer to rheumatologist |
| Limited mobility | Request specialized orthopedic evaluation |
Diagnostic processes for joint pain
Medical professionals use various diagnostic tools to understand the root cause of joint pain. These may include physical examinations, imaging studies, blood tests, and detailed medical history reviews. Be prepared to provide comprehensive information about your symptoms, lifestyle, and any previous treatments[24].
Exploring treatment options
Depending on the diagnosis, healthcare providers might recommend multiple treatment approaches. These could range from medication and physical therapy to specialized interventions like joint injections or surgical procedures. Each treatment plan is tailored to the individual’s specific condition and overall health status.
Developing a long-term management strategy
Working collaboratively with healthcare professionals allows you to develop a comprehensive joint health management strategy. This approach combines medical expertise with personal commitment to maintaining joint function and minimizing pain, ensuring a holistic approach to your overall well-being.
Frequently Asked Questions
Aim for 15-20 minute sessions with a protective barrier between your skin and the ice pack. Take breaks of at least 45-60 minutes between icing sessions to allow your skin and tissues to recover, preventing potential nerve or skin damage.
Excessive icing can actually hinder the natural healing process by restricting blood flow and potentially causing tissue damage. Follow the recommended 15-20 minute intervals and allow your body adequate time to respond between cold therapy sessions. If you experience increased pain or numbness, stop icing and consult a healthcare professional.
Chronic pain often responds better to a combination of heat and cold therapy. While ice reduces inflammation, heat helps improve circulation and relax muscles. Experiment with alternating between the two or consult a physical therapist to develop a personalized approach that addresses your specific condition.
Choose gel-based ice packs that conform to body contours, providing more consistent cold coverage. Reusable gel packs with flexible materials are ideal, as they can be molded around joints and provide even cooling. Ensure the pack has a protective cover to prevent direct skin contact and potential freezer burn.
Individuals with compromised circulation should exercise extreme caution with ice therapy. Consult your healthcare provider before attempting cold treatments, as reduced blood flow can increase the risk of tissue damage. Alternative pain management strategies like gentle compression, mild heat, or specialized massage might be more suitable.
Always use a thin towel or specialized barrier between your skin and the ice pack. Limit direct contact to prevent skin damage, and never apply ice directly to the skin. Monitor your skin during icing for signs of excessive redness, whitening, or unusual sensations, which might indicate potential tissue damage.
Reference list
- Bleakley CM, Glasgow P, MacAuley DC. PRICE needs updating, should we call the POLICE?. British Journal of Sports Medicine. 2012;46(4):220-221.
- Casa DJ, Armstrong LE, Hillman SK, et al. National Athletic Trainers’ Association position statement: fluid replacement for athletes. Journal of Athletic Training. 2000;35(2):212-224.
- Cheung K, Hume PA, Maxwell L. Delayed onset muscle soreness: treatment strategies and performance factors. Sports Medicine. 2003;33(2):145-164.
- Davidson JR, Moldofsky H, Lue FA. Treatment with cytokine antagonists in patients with fibromyalgia: a randomized controlled trial. Arthritis & Rheumatism. 2005;52(9):2775-2782.
- Devasahayam A, Vadivelu R, Acharya PT. Advanced cryotherapy techniques in sports medicine. Journal of Sports Science & Medicine. 2018;17(3):401-410.
- Dubois B, Arnold D, Banaras J. Soft tissue injuries and cryotherapy: current perspectives. Sports Medicine Open. 2016;2(1):35.
- Epstein M. Heat and cold therapy: evidence-based recommendations. Postgraduate Medicine. 2013;125(1):74-81.
- Garra G, Singer AJ, Leno R, et al. Heat or cold packs for neck and back strain: a randomized controlled trial of efficacy. Academic Emergency Medicine. 2010;17(5):484-489.
- Griefahn B, Künemund C, Golka K, et al. Melatonin synthesis: a possible indicator of intolerance to shiftwork. Journal of Pineal Research. 2002;33(1):1-5.
- Halbertsma JP, van Bolhuis AI, Göeken LN. Stretching exercises: effect on passive extensibility and stiffness in short hamstrings of healthy subjects. Archives of Physical Medicine and Rehabilitation. 1996;77(9):659-662.
- Hubbard TJ, Aronson SL, Denegar CR. Does cryotherapy hasten return to participation? A systematic review. Journal of Athletic Training. 2004;39(1):88-94.
- Juul-Kristensen B, Bojsen-Møller F. Experimental measurements of ligament strain in humans. Scandinavian Journal of Medicine & Science in Sports. 2000;10(5):320-325.
- Kalmar JM, Cafarelli E. Central fatigue and transcranial magnetic stimulation. Exercise and Sport Sciences Reviews. 2004;32(2):60-65.
- Khoshhal KI, Mir HR. Prevention and treatment of complications following pediatric fractures. Journal of Orthopaedic Surgery and Research. 2018;13(1):200.
- Knight KL. Cryotherapy in Sport and Exercise. Human Kinetics; 1995.
- Macdonald HM, New SA, Campbell MK, et al. Magnesium supplementation and bone mineral density in midlife: a randomized, placebo-controlled trial. Journal of Bone and Mineral Research. 2008;23(3):386-394.
- Merrick MA. Secondary injury after musculoskeletal trauma: a review and update. Journal of Athletic Training. 2002;37(2):209-217.
- Nedelec M, McCall A, Carling C, et al. Recovery in soccer: part II – recovery strategies. Sports Medicine. 2013;43(1):9-22.
- Noguchi K, Sakamoto N, Shigemoto T, et al. Effectiveness of cold therapy: a systematic review. Journal of Physical Therapy Science. 2014;26(5):713-718.
- Oakley ET, Pardeiro R, Powell D, et al. The effects of pitch and duration of cold water immersion on recovery from exercise-induced muscle damage. Journal of Sports Sciences. 2018;36(8):940-946.
- Okamoto T, Hirata K, Ando S, et al. Effect of heat and cold treatment on the inflammatory response after exercise. Journal of Sports Science & Medicine. 2013;12(3):442-450.
- Schaal K, Le Meur Y, Bieuzen F, et al. Recovery from exercise-induced muscle damage: cold water immersion versus passive rest. PLoS One. 2013;8(12):e82568.
- Wilcock IM, Cronin JB, Hing WA. Physiological response to water immersion: a method for sport recovery?. Sports Medicine. 2006;36(9):747-765.
- Yanagisawa O, Kudo H, Fukubayashi T. Magnetic resonance imaging evaluates the effects of cooling on muscle strain injuries. The American Journal of Sports Medicine. 2007;35(7):1216-1223.
 Mildronate capsules 500mg, 90pcs
Mildronate capsules 500mg, 90pcs  Picamilon pills 50mg, 60pcs
Picamilon pills 50mg, 60pcs  Cavinton Comfort, dispersible pills 10mg 90pcs
Cavinton Comfort, dispersible pills 10mg 90pcs  Cortexin, 10mg, 5ml, 10pcs
Cortexin, 10mg, 5ml, 10pcs